Need “Community-based” approach to failed “Command and Obey” Colombo-centric approach

Month of April 2021 here in Sri Lanka recorded very high numbers of COVID-19 cases with over one thousand and six hundred positive cases reported daily towards the end of the month.
Fatalities has now reached over 700 from 604 since Sinhala-Tamil New Year. Month of May began with a further increase and the daily number recorded was 1,923 on 03 May.
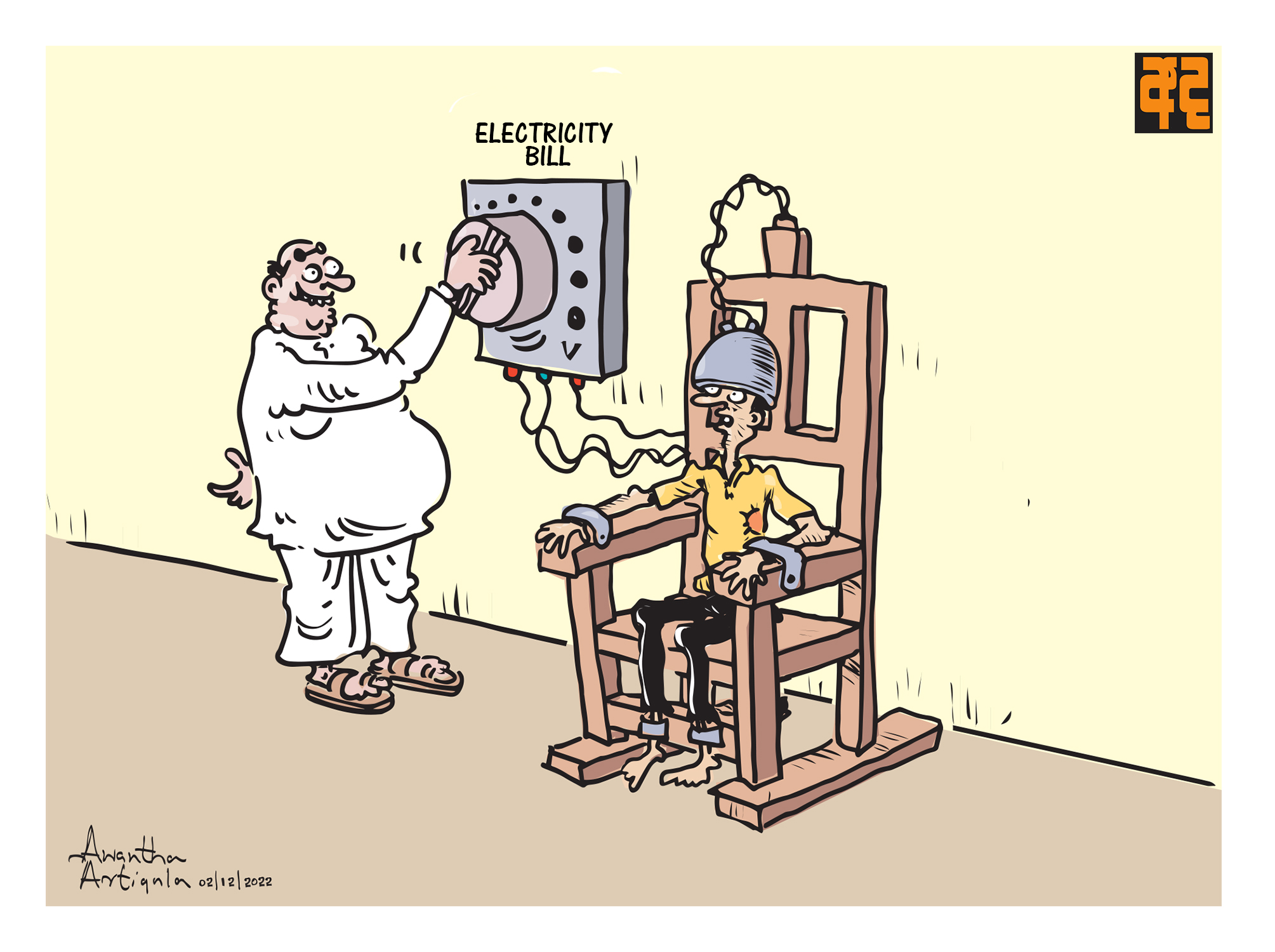
Every wave carried strict preventive instructions to follow, always issued from Colombo. They were the same precautionary methods clamped down in March 2020, thereafter given more teeth and force every time, announced through Police spokesman. Recently security forces were deployed under gazette notifications. Yet the third wave is scarier than the previous two.
Neglect of social responsibility was clearly in show with the urban affluent flocking to Nuwara-eliya for holiday fun and the religious Sinhala Buddhists trekking Sri Pada for worshiping. Blame for the rapid spread of COVID-19 virus nevertheless was on the poor and the marginalized. They were accused of “ignorant and callous disregard for preventive measures”. They remain the lot who are arrested for violations.
 Holidaymakers paid little to no attention to health guidelines as they flocked to Nuwareliya in April.
Holidaymakers paid little to no attention to health guidelines as they flocked to Nuwareliya in April.
Ironically, the post second wave continued with crowded festivals, political events, and rallies both by ruling and opposition parties creating a mindset that social life is “normalising”. This gave room for the third wave with weekend buffets, night outs with dinners and dances for the urban elite. It was predicted with Sinhala-Tamil New Year shopping and festivities the outbreak could be far worse than the two before. Neglect of social responsibility was clearly in show with the urban affluent flocking to Nuwara-eliya for holiday fun and the religious Sinhala Buddhists trekking Sri Pada for worshiping. Blame for the rapid spread of COVID-19 virus nevertheless was on the poor and the marginalized. They were accused of “ignorant and callous disregard for preventive measures”. They remain the lot who are arrested for violations.
Meanwhile education from pre-school to university hit a new low. Re-opening and closing of both public and private schools during the past year have been erratic to say the least, ruining the future of over 4.5 million students. Education has become intolerably chaotic with totally alien “online teaching” dumped on students and teachers without any pre planning and preparations. So are universities and higher education institutes. One joked, in Sri Lanka even the Open University remains closed.
Rural economy is dragged on for survival. Most Sunday fairs have lost their vendors and customers, with less transport available. Produce collectors do not come to villages as before and cashflows have shrunk. Small time shop owners do not have retailers coming their way to sell small items that usually run fast. It is a multiple catastrophe that eats into each other. Everything points to a fast-deteriorating situation with growing uncertainty and hopelessness.
In the formal economic sector, factory workers are insecure with employers wanting to maximise profits using COVID-19 pandemic crisis to reduce numbers in their workforce too. Added is neglect of establishing preventive measures in factories by employers. This has led to the closure of a factory in Ridimaliyedda, where over 175 employees were tested positive on 03 February (2021) out of 2,500 workers. In Katunayake FTZ and in other places, factories face closure with fair numbers of workers tested often reported as positive.

Need for increased numbers of beds, ventilators, oxygen and ICU facilities have created more uncertainty in society. They also create a new demand for more special trained nurses and technical staff.
Rapidly increasing positive and fatality numbers have brought heavy pressure on all hospital staff and a scarcity on essential human and material resources. Need for increased numbers of beds, ventilators, oxygen and ICU facilities have created more uncertainty in society. They also create a new demand for more special trained nurses and technical staff. On the side lines, there is confusion over vaccination programmes coming almost to a halt.
There are two very urgent demands right now that have to be met. Keeping vaccinations on hold for now, one is to treat the already hospitalised and incoming COVID-19 patients and to have all necessary resources adequately arranged for them. That being the short-term urgent response, the second and the long-term need is to urgently bring down positive numbers. This requires a well-defined and detailed COVID-19 combat plan for at least the next 06 months.
Whole approach in this Colombo centric “Command and obey” approach is based on beds, hospitals and medical practitioners only valuable in a “curative healthcare” system. COVID-19 prevention is not about accommodating increasing numbers of COVID-19 cases for hospitalised treatment. It is about seriously reducing infections in society.
Planning for such requires a wholly different a-political approach to what has been the practice so far; decisions politically made in Colombo with enforcement agencies given instructions to implement. Present “command and obey” approach with no planning proper has proved a total failure with two waves disrupting socio-economic life within 09 months after the first during March-May 2020.
The “Command and obey” approach has also had provincial and local political interferences. Whole approach in this Colombo centric “Command and obey” approach is based on beds, hospitals and medical practitioners only valuable in a “curative healthcare” system. COVID-19 prevention is not about accommodating increasing numbers of COVID-19 cases for hospitalised treatment. It is about seriously reducing infections in society.
To date with this present approach, people do not see reasons for co-operation when authorities are not seen as responsible decision makers. When people are treated as “culprits” for getting infected. A change therefore is a must. We need a new community healthcare approach in controlling the COVID-19 spread.
Why people at present avoid providing information and why infected people sometime go missing is because the present “command and obey” approach has created a repressive stigma around infected persons and families. Often treated as social miscreants.
For a community-based preventive healthcare programme the PHI and the FHSO are two extremely important field health workers, who should be given total responsibility in COVID-19 preventive work. People know them in their work areas. It is important for people to trust officers who come to them, to provide all required information. Why people at present avoid providing information and why infected people sometime go missing is because the present “command and obey” approach has created a repressive stigma around infected persons and families. Often treated as social miscreants.

Unfortunately, larger majority of the people are totally unaware of the experience and the role of Public Health Inspectors (PHI) and of Family Health Service Officers (FHSO – Midwives decades ago) in totally eradicating epidemics like Malaria, Measles, Filariasis, Polio and other communicable diseases. Most have forgotten how sanitary facilities, personal hygiene, maternal and child health came to be improved beyond Asian levels during 50’s and 60’s, irrespective of the colour of the ruling party.
PHIs were held responsible for “gaining confidence and co-operation of the people, investigate cases of communicable disease, keep contacts under surveillance, take appropriate action to prevent further spread of disease and assist in tracing contacts, assist Specialized Campaigns in disease control activities, regularly inspect houses and advise on the requirements of sanitary latrines, water supply, refuse disposal, light and ventilation” in a detailed duty list of 21 items.
Added was that of FHSOs, the most dedicated service in the whole public service. They work at grassroots level and keeps the infant and maternal mortality rate lowest in Asia at a beggarly per capita cost of around 125 US dollars for public health, per annum. An Al Jazeera journalist who in early 2016 covered the work trail of a FHSO reported “the care is highly personal” and how “mothers stop her on the street and on the stairs for a quick word and help interpreting test results…..”
In a short write up titled “Meet the Sri Lankan Midwives bringing miracles to families” in the “Med Tech” online notes, “A Sri Lankan midwife helps newlyweds with family planning, provides prenatal care and ensures that high-risk pregnancies receive specialist care. Within two months after a delivery, she’ll visit the mother and baby four times to perform thorough check-ups.” All this says, they are firmly on the ground with people.
In a complete shift from “command and obey” Colombo centric curative healthcare approach to a community-based preventive healthcare system, these field level health staff are indispensable. They have to be brought in as responsible officers under the MOH. The MOH office should be made the community-based “COVID-19 preventive unit” in the area that works in alliance with the GN of the division. This trio, the PHI, FHSO and the GN should be given a quick medical briefing on COVID-19 pandemic, its variants, symptoms and preventive measures including quarantine procedures at home, restricting common quarantine centres to “visitors” and “returning expatriates”.
The total plan to be accompanied by a detailed working programme should be designed by few very selective Community Healthcare experts, with PHI’s and FHSO’s union representatives in attendance. The policy plan should include,
- MOH offices to be established as “COVID-19 preventive Units” under the MOH, with PHIs and FHOs given responsibility to monitor all households in their respective areas (roughly about 1,000 to 1,500) supported by the GNs.
- all field staff in MOH offices and GNs should be provided with PPE, masks, face covers and necessary resources immediately.
- a Special Duty Allowance (SDA) not less than Rs.5,000 should be given as incentive for strenuous all day work and health risk.
- Socio-economic life in the district should be regulated and monitored under the District Secretary, supported by Divisional Secretaries and all MOH in the district.
- Special plan should be included for reopening of schools during the next 06 months beginning 01 June and maintenance of safe public commuting, with special attention given to public employees including teachers.
- Employers should be instructed to immediately arrange for PCR testing of all factory employees and provide transport for their factory employees within districts.
- District Secretariat should update and maintain a District data-base made available as open source for all Citizens
This in short is a proposal for immediate consideration as the present Colombo centred, curative healthcare approach is being proven a total failure.
Proposals for increasing PCR testing, requesting more beds, oxygen, ICU facilities are immediate necessities to meet the chaos that is being heaped on society, but no answer to the accelerated spread. In short, change of frames for the outdated lenses, provides no new clear vision for the future.
Kusal Perera
2021 May 05